Plantar fasciitis treatment advice from a podiatrist with over 10 years experience treating heel pain as well as 8 years teaching podiatry students about heel pain. If you have plantar fasciitis, this ones for you. But if you’re not sure what’s causing your heel pain start with the free online heel pain test. It takes less than 1 minute to get your results.
At PridePlus Health one of the most common presentations we see is our beloved community suffering with is heel pain. People literally begging for the best plantar fasciitis treatment every day. When we have sore heels, the impact on our lives is immense so there’s often very little wiggle room with plantar fasciitis treatment.
We want to get better, and we want it now.
Let’s take you through effective, evidence based, fast and personal plantar fasciitis treatment options.
But first, what is plantar fasciitis again?
Background Info: Plantar Fasciitis 101
Plantar fasciitis is the old school name for a very modern problem. Heel pain where the plantar fascia, a strong and stretchy sinew (kinda like a ligament crossed with a tendon) called the plantar aponeurosis (or plantar fascia) becomes overworked and sore.
In the past it was called plantar fasciitis or policeman’s heel. Nowadays we go by plantar fasciopathy… a more modern term that describes the pathology more accurately as it’s not really inflammatory. This is what the -itis suffix in plantar fasciitis infers. We now know it to be a chronic overload, hence -opathy as the more correct suffix in 2020 and beyond.
You can check out our super in depth guide on plantar fasciitis (plantar fasciopathy) here.
For the basics, things that are really useful when commencing plantar fasciitis treatment the key points to remember are.
- The plantar fascia loves tensile loading (being pulled)
- It hates compression loading (being squished or twisted)
- It’s really, really strong. In cadaver workshops us podiatrists find it almost impossible to cut with surgical scalpels.
- It can be sore when it’s overworked due to
- Too much of the compression it doesn’t like (often only takes a little of this)
- Too much of the tensile loading it does like (takes A LOT of this to get sore)
- Too little capacity to do the work. Diabetes, stress, some medications, obesity all limit the capacity of our plantar fascia to tolerate load.

What Does Plantar Fasciitis Feel Like?
Pain is subjective, we all feel things differently but there is some consistency with plantar fasciitis.
- Pain under your heel bone or just into the start of the arch.
- Symptoms are usually (not always) worse first thing in the morning or if you get up after a rest
- The pain tends to warm up a little with movement and then get worse with prolonged loading
- It’s often sharp initially, achey-throb like symptoms later on.
Anatomy Of The Plantar Fascia
Picture a trident, you know, those big fork looking weapons that Neptune and Poseidon carried around?
The plantar fascia starts at the base of the heel bone, the calcaneus. Pretty much smack bang centre of the bottom of the heel. If you have plantar fasciitis then around 60% of the time it’s this origin of the plantar fascia which gets really sore. You can probably locate it with a gentle press on your sole at the heel.
From this origin it spreads and has connections to the metatarsophalangeal joints (MTPJ’s), also known as the joints that make up the ball of the foot.
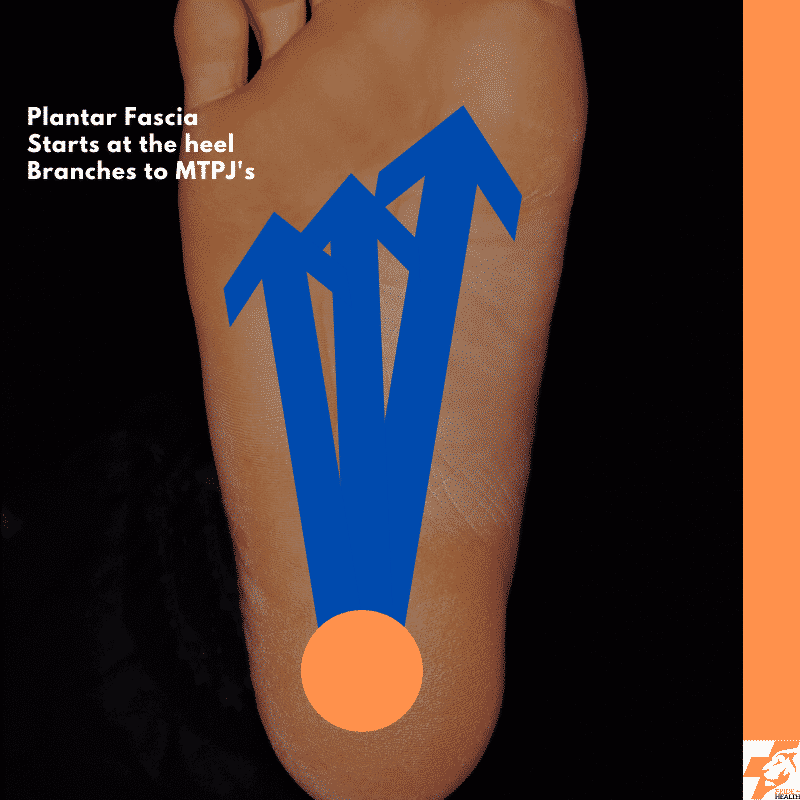
If you can imagine just looking at the plantar fascia without the skin and fat pad over the top of it it looks very white and shiny, flat too. A taut and strong support for our feet.
When we walk, the plantar fascia is pulled and gets longer (that tensile loading it loves). Eventually as we lower ourselves down to the ground the plantar fascia as well as our balance muscles in our leg hold on tight to keep our foot steady.
Then when we lift off and spring forwards our plantar fascia provides some extra support around the ball of the foot to encourage us to use our big toe and move forwards. If we have some underlying strength imbalance or maybe a slightly different from the normal bone structure to our feet we sometimes twist our heel at this time. If you twist it in or out while pushing off this can lead to compression within the flat plantar fascia.As you know, the plantar fascia doesn’t like this much at all.
Would like to read more on all the types of fascia in our body? Check out our anatomy series on fascia here.
Who Is Most Likely To Get Plantar Fasciitis?
Anyone who asks their plantar fascia to do more than it can handle will suffer with plantar fasciitis. In saying that, some people are more likely.
- The Demanding Foot: Very high demands from elite or sub elite athletes can lead to a painful plantar fascia. Same too if work demands are really high. Remember that old name? Policeman’s heel? Back when the plod used to plod the streets before segways and patrol cars a lot of coppers used to get plantar fasciitis from all that walking.
- The Sedentary Foot: If you don’t use it, you lose it. If your foot isn’t active then the plantar fascia and muscles which support you lose their strength and then it really doesn’t take much standing on them before they get sore
- The Diabetic Foot: Unfortunately those with diabetes, even brilliantly controlled are at a higher risk of suffering with plantar fasciitis.
- The Stressed Out Foot: Stress raises cortisol levels in the body which is a hormone which impacts tissue health. If you’re constantly over stressed then just like a skin break out – your plantar fascia can break out in pain too.
- The Funny Shaped Foot: We’re not talking funny haha, more funny as it’s a bit different. Higher arched feet are more likely to have increased compressive loads placed on the plantar fascia. The opposite is true of lower arched or flat feet. These feet tend to put more tensile load on the plantar fascia.
- The Pregnant Foot: Congratulations Debbie! But carrying the extra weight of bub means extra work for the plantar fascia. Couple this with the release of a hormone known as relaxin which loosens up ligaments and all of a sudden the plantar fascia is being really worked.
- The Older Foot: Sorry Nan, I have to be an ageist here. The older we get, the less capacity our plantar fascia has.
- The Shoddy Shoe’d Foot: While it’s never 100% the shoes fault, some shoes greatly contribute to plantar fascial loading whereas others can decrease it.
How To Diagnose Plantar Fasciitis
Clinically a diagnosis of plantar fasciitis is made by your podiatrist. It’s a combination of history, anatomy, social and medical factors and then a physical examination. Usually some active tests of strength, balance and a gait assessment are conducted as well.
An accurate diagnosis is important as there are a lot of other things that can go wrong around the plantar fascia which can lead to heel pain.
They are
- Fat Pad Herniation/Inflammation
- Baxter’s Nerve Entrapment
- Calcaneal bursitis
- Plantar fibroma
- Achilles tendinopathy
- Haglund’s deformity
- Calcaneus Stress Fracture
- Quadratus Plantar Strain or Tear
- L5/S1 Radiculopathy (Nerve Root Entrapment)
Do You Need A Scan Before You Start Your Plantar Fasciitis Treatment?
A scan is not usually part of plantar fasciitis treatment as the diagnosis is a clinical one. In saying that there are often unique and extenuating circumstances where you might get an ultrasound or MRI.
In Australia ultrasound imaging is rebateable and referrable by your PridePlus Health podiatrist so if it’s looking like this is needed we can arrange that for you. An ultrasound might be called for if there is a clinical suspicion of a plantar fibroma as this would change your plantar fasciitis treatment pathway.
An MRI is rarely used but at times called for to check out some of the deeper tissues in the foot and ankle that an ultrasound just can’t reach.
Plantar Fasciitis Treatment – Settling The Pain
Usually the first step to plantar fasciitis treatment is settling the pain. Depending on the exact causative factors you have, different treatments modalities will work better for you than the next person.
Plantar Fasciitis Treatment – Strapping
Strapping the foot to support the plantar fascia will lead to an immediate reduction in load and pain. In clinic it usually leads to a dramatic “Oh wow” moment where what was previously very sore is now pain free or close to it.
We’ve written a whole post (+ video) on the 4 strap method to strap your foot for plantar fasciitis.
There are many ways to strap a foot as part of your plantar fasciitis treatment plan however this one is the easiest and most repeatable at home. I’ve taught hundreds of podiatry students and thousands of plantar fasciitis sufferers this technique over the years.
What you will need is a RIGID sports tape. Definitely not kinesio tape for this one. Ideally the 38mm tape works best but you can get away with the 20mm or 50mm tapes too at a pinch.
And as father always used to say, measure twice, cut once. You don’t want to be strapping your feet to your hand with extra lengths.
The 4 Strap Method
- Cut or tear two 5 cm lengths of tape. These will be the anchor points.
- Cut or tear two lengths of tape that will go from the back of your heel where your achilles reached the heel bone, to your 1st MTPJ. That’s your big toe joint at the ball of the foot.
- Place an anchor tape piece at the back of your heel where the achilles reaches your heel bone.
- Now run one of the longer strips from that anchor underneath your foot, past your arch and get ready to stick it to your big toe. Just before you stick it down you need to bend your big toe back/up towards you (called dorsi-flexion). Now stick that tape down. You should get your arch being quite high looking like a bow and the tape forming the bow string underneath.
- Repeat 4.
- Repeat 3.
Pop on a sock and give the strapping tape a gentle massage to help the glue stick to the skin. The strapping tape will be even more comfortable if worn with an appropriate shoe.
Plantar Fasciitis Treatment – Orthotics
Orthotics are those comfortable devices that sit inside shoes to give you more support. For plantar fasciitis treatment orthotics come in two categories. Custom Foot Orthotics and Prefabricated Foot Orthotics.
Depending on your foot, shoes, and what’s causing your plantar fasciitis a prefabricated device might be a really successful tool to knock those painful initial symptoms on the head.
Often we need to think more long term or more specific than what a prefabricated orthotic can offer us. Maybe we need to fit an orthotic into a footy boot or dress shoe? Maybe the left and right feet are wildly different from each other?
In these cases a custom foot orthotic is prescribed and 3D printed to provide that support for pain relief.
Plantar Fasciitis Treatment – NSAIDs
Are short for nonsteroidal anti-inflammatory drugs. Ok, nurofen and voltaren are the main NSAIDs we think about or have sitting in the cupboard.
NSAIDs can sometimes provide a small amount of symptom relief (think 1-2 points on a 10 point pain scale) in the short term. They do come with side effects however and for those with kidney disease or gastro-intestinal risks should definitely avoid them.
A trial of topical diclofenac (voltaren gel) rubbed directly into the sore area of the heel and arch can be a good way of getting a small window of pain relief.
You cannot continue this long term and also it makes strapping difficult to complete as the tape doesn’t stick well to the creamed up feet. If I had my choice of strapping or topical NSAIDs it would be strapping for me every day of the week, and twice on Sunday.
Plantar Fasciitis Treatment – Massage
We all love a massage! Well, most of us do. As does most of our plantar fascia. Self love with some self massage is a simple way to get some short term pain relief.
For a detailed post on plantar fasciitis massage techniques you can read all about the various options here.
For the most basic plantar fascia massage you can do this by sitting cross legged and rubbing your thumbs into your plantar fascia through the underside of your foot. Start with firm pressure to feel some initial discomfort (not pain) is safe.
Just like other massages it’s always better to get some love from another person. A physio sports massage working on the calf muscles is a great way to lead to heel pain relief and is an important consideration for plantar fasciitis treatment.
The exact understanding of why a sports massage into the calves is helpful is not clear. There are some effects on our central processing unit (our brains and spinal cord) with massage here. Also, relaxing the calf muscles even in the short term will lead to a reduction in plantar fascial tension. There’s also theories relating to fascial chains throughout our body.
In summary, self massage is good, physio sports massage in the area is even better.
Plantar Fasciitis Treatment – Shoes
Us podiatrists love talking shoes but I’ll keep this super simple here. The best shoes for plantar fasciitis is really a whole other post which you can read here.
Some shoes make our plantar fascia work harder. Very flexible soled shoes and very flat shoes all increase the lever arm that the ground pushes on us when we are walking. If they don’t have any extra support through the midsole then that work gets done by our leg muscles and plantar fascia.
Also when we increase the height of the heel of our shoes our plantar fascia loading reduces a touch as well.
So you should wear your shoes that your plantar fascia feels the best in. Ideally they will have a slight heel and pass the twist test.
Plantar Fasciitis Treatment – Exercises
Plantar fasciitis treatment starts, middles and ends with exercises. As the plantar fascia is a soft tissue it can be trained really well to tolerate more load. Also, some exercises can give us pain reduction too.
The initial phase of exercise for your plantar fasciitis treatment will vary person to person and foot to foot. Let’s use a pretend plantar fasciitis sufferer named Jenny as an example. Jenny has plantar fasciitis on her left foot only.
Jenny’s Exercise Plan
Left Foot (The sore one)
- A standing isometric calf hover on just her left side.
- Jenny set’s up with a rolled towel under her toes and the ball of her foot on a step.
- Staying still, not rising or lowering Jenny is aiming to get 60 seconds of isometric loading done.
- Repeat this 3 – 5 times
Right Foot (The good one)
- Same starting position as the left however on the good foot Jenny is going to do 3 – 5 sets of calf raises
- This is where Jenny rises up onto her toes (on the towel) and then lowers back down again.
Why is Jenny doing these exercises on both feet if only one is sore with plantar fasciitis? A little thing called cross education! We know that when we exercise one side of our body, the other side gets a little stronger too. It’s a great tool or magic trick even for unilateral (one sided) pathology.
Plantar Fasciitis Treatment – Activity Modification
This part of the treatment is avoiding activity that makes things worse. It could be cutting down the running distance, reducing the time on your feet at work, changing your exercise class at the gym. Sometimes it’s not possible, that’s fine. We just do more of the other treatments then.
Plantar Fasciitis Treatment – Fixing The Pathology
The second phase of plantar fasciitis treatment is fixing or rehabilitating the pathology. During this phase we have gotten the symptoms in check (usually settled but not “perfect”). The work shifts to getting that plantar fascia strong and stretchy again and making those calf muscles even stronger.
Fixing Plantar Fasciitis – Exercises
A progression of where the initial exercises started is in order. What makes this even easier to follow is that the progression is just moving towards what was being done on the good leg in the initial phase!
Let’s consider Jenny again. Remember her with the sore left plantar fascia? During the fixing phase Jenny will start completing her calf raise exercises on her left side now that she was previously doing on her right.
On the right side incorporating some higher level work with lunges, squats, clam walks and therabands will be on the menu.
Fixing Plantar Fasciitis – Orthotics
During this phase orthotics become more valuable as they don’t need to be reapplied daily like strapping tape. They can just sit there and do their job while we focus on what we need to do. Exercise.
Fixing Plantar Fasciitis – Shoes
Just like in the acute phase shoes are still important factors to consider. At this point of your plantar fasciitis treatment you might be able to move to less supportive shoes at times. That would be if:
A) You are not doing as much physical activity at that time.
Or B) You have some extra support from your orthotic.
Fixing Plantar Fasciitis Lifestyle Checklist – Sleep, Diet, Stress
To rehabilitate any injury we need to be getting enough sleep. During sleep our body goes through a general clean out and de-clutter. If we’re not sleeping enough we don’t get enough repair time to fix our plantar fascia for good and we get an increase in cortisol in the body. Both of these delay and in severe cases prevent plantar fasciitis treatment from being successful.
Sleep tight and sweet dreams for your sore heels sake.
Diet is also important for injury rehabilitation and outside the scope of a podiatrists playbook. Just remember to be getting plenty of good, healthy vegetables by the plate load and you should be on the right path.
Seeing a dietitian would be the best course of action if you’re thinking your diet might need a tweak to allow your plantar fascia to repair.
Just like a lack of sleep, excess stress from work or at home can lead to more of that free flowing cortisol hormone in our body. A little bit of cortisol is good, too much is not. Take time to meditate, do yoga, see a psychologist or talk with friends if your stress levels are too high.
Plantar Fasciitis Treatment – The Sometimes For A Rare Cases Options
Steroid Injections For Plantar Fasciitis
Steroid injections (also known as cortisone injections) have gone in and out of favour over the years. There’s plenty of evidence that a steroid injection into the plantar fascia will lead to an immediate symptom reduction.
BUT.
And this is a big but.
Steroid injections are no more effective in treating plantar fasciitis than other measures which come WITHOUT all the nasty risks and side effects. The main risks are rupture of the plantar fascia (you don’t want that), infection (you really don’t want that) and an increase in pain (pass thank-you).
There’s also the systemic effects of a steroid injection. If you have diabetes (which is a risk factor for plantar fasciitis so a lot of sufferers do) then an injection will play havoc with your blood sugar management.
If you’re considering a steroid injection it’s best to have a really long and thorough discussion with your podiatrist first.
ECSWT For Plantar Fasciitis
The shockwave gun! The use of extra corporeal shock wave therapy for plantar fasciitis is indicated for pain that has been present greater than 6 weeks.
Surgery For Plantar Fasciitis
Considered a last resort treatment for plantar fasciitis. Surgery is rarely required however rare things still exist. Depending on the person and the chronicity of the plantar fasciitis, surgery might involve lengthening of the plantar fascia, the achilles or a general “clean out” of the plantar fascia.
In Summary
Plantar fasciitis treatment is one of our most common requests at PridePlus Health. Helping people overcome their sore heels is absolutely one of the most rewarding aspects of being a podiatrist. If you have plantar fasciitis or know someone please share this post with them. The more people we can help with their plantar fasciitis treatment, the happier I will be.
Disclaimer
This article is general advice around plantar fasciitis treatment from an experienced podiatrist. It is not specific to any person or heel pain sufferer and should not be used in place of an assessment with your podiatrist.
If you need plantar fasciitis treatment you can book online with our podiatry team here.