Plantar Fasciitis Treatment
Sharp morning heel pain? We can fix that.
Plantar fasciitis is one of the most common causes of heel pain — and one of the most treatable.
That thick band of tissue under your foot has become irritated or damaged. The stabbing pain with your first steps in the morning, the ache after sitting or standing too long — it doesn't have to be your new normal. At Pride Podiatry, we diagnose the root cause and build a treatment plan that gets you back on your feet — comfortably.
Book Your Podiatry Session
Do you think waiting longer will help overcome your foot and ankle pain? Don't put off looking after yourself today and your body will thank you tomorrow.
Or call us on 0399 754 133
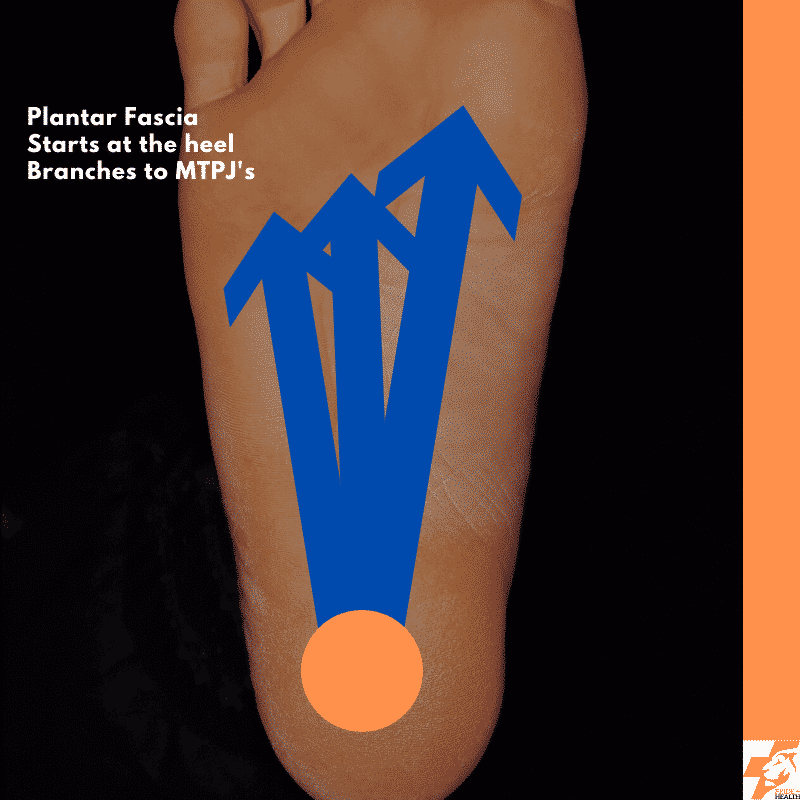
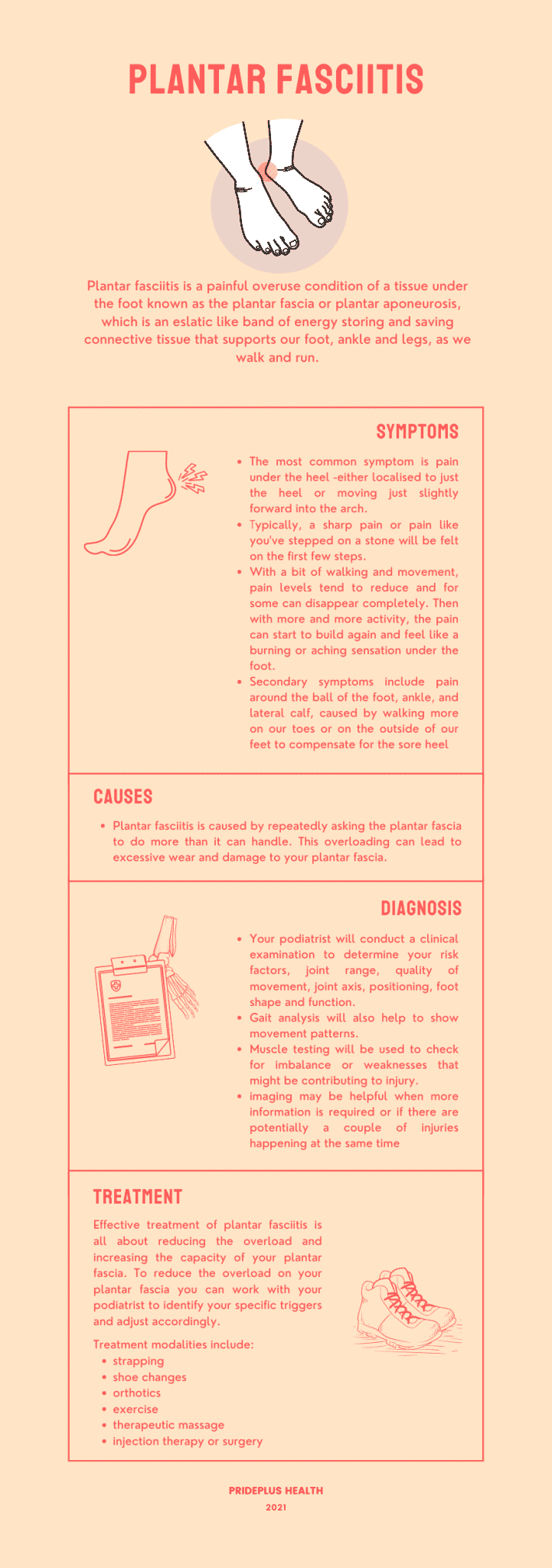
What Is Plantar Fasciitis?
Understanding what's happening in your foot is the first step to fixing it.
Common Symptoms
Sharp or burning heel pain with your first steps in the morning
Pain that returns after sitting or standing for a while
Pain that improves with movement but comes back after rest
Stiffness and aching through the arch of the foot
Demand Exceeds Capacity
Plantar fasciitis happens when the load on your plantar fascia exceeds what it can handle. Think of it like a rope — it’s strong, but if you keep pulling harder than it can tolerate, it starts to fray. The fix isn’t just reducing load — it’s building the tissue’s capacity to handle more.
Tension Load
Your plantar fascia works like a rubber band connecting your heel to your toes. Every step you take stretches it under tension. When you’re walking, running, or just standing, this tensile loading adds up — and if the tissue isn’t strong enough, it breaks down.
Compression Load
Your heel tilts and compresses the tissue where it attaches to the bone. Inversion and eversion of the foot can increase this compression, adding another layer of stress. Understanding both tension AND compression is key to effective treatment.
Risk Factors
How We Diagnose It
Diagnosis is clinical — a skilled podiatrist can usually confirm plantar fasciitis without imaging. We don't guess.
Detailed history — when it started, what makes it worse, what you’ve tried
Physical examination — palpation, joint range of motion, foot shape assessment
Gait analysis — how you walk and how force moves through your foot
Capacity testing — calf raise power and endurance to measure your baseline
Imaging if needed — MRI or ultrasound (not X-rays) for complex or persistent cases

How We Treat Plantar Fasciitis
Our approach follows a proven framework: reduce the load, then build your capacity. Not just rest and hope.
Assessment & Root Cause
Gait analysis, capacity testing, and thorough examination to find the actual cause — not just treat the symptoms.
Load Reduction
Strapping tape, footwear changes, and custom orthotics to bring the load down below what your tissue can handle — so it can start healing.
Capacity Building
Structured calf raise programs to progressively strengthen the tissue. This is the most important part — building your fascia’s ability to handle load again.
Shockwave Therapy
Acoustic waves stimulate healing in damaged fascia tissue. One of the most effective treatments for chronic cases. Included in your consultation.
Dry Needling & Massage
The 1-per-centers that support your recovery — soft tissue work, dry needling, and laser therapy to complement the main treatment.
What Doesn’t Work
Calf stretching alone won’t fix plantar fasciitis. Cortisone injections and surgery are only considered when conservative treatment has genuinely failed.
What to Expect
60-Minute Initial Consultation
No rushed appointments. We take a full hour to understand your pain, assess your biomechanics, and build a treatment plan that actually works.
Your Consultation Includes
- ✓Full biomechanical assessment and gait analysis
- ✓Calf raise power and endurance testing
- ✓Clear diagnosis and explanation of root cause
- ✓Personalised treatment plan with exercises
- ✓Shockwave or laser therapy if needed (included)
The Outcome
You'll leave with a clear understanding of what's causing your plantar fasciitis and a roadmap to get rid of it — for good.

Free Email Course
The Heel Pain Reset
Not ready to book? Start with our free email course. The Heel Pain Reset walks you through the key steps to understanding and overcoming plantar fasciitis — delivered straight to your inbox.
Sign Up Free →Plantar Fasciitis Treatment Pricing
Transparent pricing. No hidden fees. Shockwave and laser therapy are included in your consultation.
Initial Consultation
From $190
60-minute comprehensive assessment, diagnosis, and personalised treatment plan
Custom Orthotics
From $349
Precision-designed custom orthotics tailored to your feet and your needs
Shockwave & Laser
Included
Shockwave therapy and laser therapy are included in your consultation — no extra charge
Frequently Asked
Questions.
Is this definitely plantar fasciitis?
+Not always. Heel pain can come from several different conditions, and misdiagnosis is common. That’s why we do a thorough clinical assessment — history, physical exam, gait analysis, and capacity testing — to confirm the diagnosis before starting treatment. If needed, we’ll refer for MRI or ultrasound (not X-rays, which don’t show soft tissue well).
Will I need orthotics?
+Not necessarily. Orthotics are one tool in the toolbox — they’re great for reducing load on the plantar fascia while you build capacity, but they’re not the right answer for everyone. We’ll only recommend them if they’re genuinely going to help your specific situation.
Can I keep working or training?
+In most cases, yes — with modifications. The goal is to reduce load to a manageable level, not to stop you doing everything. We’ll help you figure out what you can keep doing safely and what needs to be dialled back temporarily.
Does plantar fasciitis go away on its own?
+Sometimes mild cases settle, but most people who “wait and see” end up with a chronic problem that’s much harder to fix. The sooner you get the right diagnosis and start a structured plan, the faster you’ll recover.
How long does it take to heal?
+If you’ve had it for less than 6 weeks, you’ll likely see significant improvement within a few weeks of proper treatment. If it’s been months or years, expect a longer road — chronic plantar fasciitis takes more time because the tissue has been damaged for longer. Either way, the key is getting started with the right plan.
Can I wear shoes while recovering?
+Absolutely — in fact, wearing the right shoes is part of the treatment. We’ll advise you on which shoes help reduce load on the plantar fascia and which ones are making things worse.
What does plantar fasciitis treatment cost?
+Your initial 60-minute consultation is from $190. This includes a full biomechanical assessment, diagnosis, and personalised treatment plan. If orthotics are recommended, they start from $349. Shockwave therapy and laser therapy are included in your consultation — no hidden extras.
What Our Patients Say
Richard Taylor
"I highly recommend Jamie Allan for excellent treatment and rehab for foot/heel issues. Combines an in depth science and research approach with technical knowledge to guide treatment that works!"
Wey
"Had a good experience with Jamie Allan, he has a very good way of explaining things and helped me well. Reception was great too!"
Lee Hendy
"Had a consult with Jamie and he couldn’t have been more helpful. Figured out what was wrong straight away & gave me practical takeaways."
Golsa Dokmechin
"It was my first experience visiting a podiatrist but I can say Ella is very professional, knowledgeable and friendly. I highly recommend them."
Grace Rosebirch
"Tim is great, a wealth of knowledge and explained everything to me so I knew how to prevent any future issues as well as providing immediate care."
Brenton Hunt
"Tim and his team are the best. Would never go anywhere else!"
Jack Stanway
"Tim is awesome. Clearly very knowledgeable and at the top of his field but also just a great guy. Explained everything thoroughly."
Alex Howe
"Tim is a great podiatrist. He is extremely knowledgeable and passionate about helping patients recover from injuries. Highly recommend!"
Richard Taylor
"I highly recommend Jamie Allan for excellent treatment and rehab for foot/heel issues. Combines an in depth science and research approach with technical knowledge to guide treatment that works!"
Wey
"Had a good experience with Jamie Allan, he has a very good way of explaining things and helped me well. Reception was great too!"
Lee Hendy
"Had a consult with Jamie and he couldn’t have been more helpful. Figured out what was wrong straight away & gave me practical takeaways."
Golsa Dokmechin
"It was my first experience visiting a podiatrist but I can say Ella is very professional, knowledgeable and friendly. I highly recommend them."
Grace Rosebirch
"Tim is great, a wealth of knowledge and explained everything to me so I knew how to prevent any future issues as well as providing immediate care."
Brenton Hunt
"Tim and his team are the best. Would never go anywhere else!"
Jack Stanway
"Tim is awesome. Clearly very knowledgeable and at the top of his field but also just a great guy. Explained everything thoroughly."
Alex Howe
"Tim is a great podiatrist. He is extremely knowledgeable and passionate about helping patients recover from injuries. Highly recommend!"
Remy
"First time seeing a podiatrist in Australia and glad I chose Tim! Addressed all my concerns and made me feel comfortable."
Sara Khorasani
"Tim was absolutely awesome. Thorough, clear explanations, and an evidence-based approach with targeted exercises. Highly recommended."
Ollie Wilson
"After a quick assessment, Tim diagnosed the problem and got me back playing footy pain free. Very professional!"
L
"Thorough assessment, proper diagnosis, exercises and new orthotics. A relief to be validated. Thoroughly recommend Pride Podiatry!"
Michael Chen
"Fantastic experience with the whole team. They really take the time to understand your issues and provide personalised treatment plans."
Sophie Williams
"Been coming here for months now and my plantar fasciitis is almost completely gone. Tim really knows his stuff!"
David Park
"The best podiatry clinic in Melbourne. Professional, friendly, and results-focused. Can’t recommend them highly enough."
Emma Johnston
"Finally found a podiatrist who listens and actually helps. My running injuries are a thing of the past. Thank you Pride Podiatry!"
Remy
"First time seeing a podiatrist in Australia and glad I chose Tim! Addressed all my concerns and made me feel comfortable."
Sara Khorasani
"Tim was absolutely awesome. Thorough, clear explanations, and an evidence-based approach with targeted exercises. Highly recommended."
Ollie Wilson
"After a quick assessment, Tim diagnosed the problem and got me back playing footy pain free. Very professional!"
L
"Thorough assessment, proper diagnosis, exercises and new orthotics. A relief to be validated. Thoroughly recommend Pride Podiatry!"
Michael Chen
"Fantastic experience with the whole team. They really take the time to understand your issues and provide personalised treatment plans."
Sophie Williams
"Been coming here for months now and my plantar fasciitis is almost completely gone. Tim really knows his stuff!"
David Park
"The best podiatry clinic in Melbourne. Professional, friendly, and results-focused. Can’t recommend them highly enough."
Emma Johnston
"Finally found a podiatrist who listens and actually helps. My running injuries are a thing of the past. Thank you Pride Podiatry!"
Stop the morning hobble. Start healing.
Book your plantar fasciitis consultation today and take the first step toward pain-free mornings.
Book Now →