Plantar Fasciitis (or 'plantar fasciopathy')

Having plantar fasciitis, also known as plantar fasciopathy or plantar fasciosis is not fun. Get up in the morning, bang, sore heel. Going for a run? Sore heel. Getting the kids off to school? Sore heel.
We build so much of our busy lives around being active and on our feet. When heel pain from plantar fasciitis strikes there’s a constant and frustrating reminder that something wrong is happening with your foot. It’s no surprise that research has found links between chronic plantar fasciitis and depression.
As podiatrists, physios and exercise physiologists we’re incredibly passionate about living active and healthy lives. We know that having plantar fasciitis is not all doom and gloom. When prepared with the facts and a personalised treatment plan you’ll be all set to overcome your heel pain and achieve your goals.
What is Plantar Fasciitis?
Plantar fasciitis is by far the most common musculoskeletal injury of the foot and ankle which we see in our podiatry clinics. More than 10% of Australians will suffer from plantar fasciitis in their lifetimes.
Quite simply, plantar fasciitis is a painful overuse condition of tissue under the foot known as the plantar fascia or plantar aponeurosis. The plantar fascia is an elastic-like band of energy storing and saving connective tissue which provides support to our foot, ankle and leg as we walk and run.
With every step, the plantar fascia is pulled taut, as the arch lowers from its resting position. This tension in the plantar fascia provides support and balance for the leg, with little metabolic cost. Unlike our muscles which require significant fuel (in the form of carbohydrates) to provide tension and contraction, the plantar fascia is much less energy-intensive.
In this way, with each step, we're able to efficiently load up our plantar fascia, get some support and balance, and spring forwards onto the next stride.
So when our plantar fascia is overworked it can lose some of these properties. The ability to store and support the foot is impaired and pain is often present.
As the causes of plantar fasciitis are varied, we've written over a dozen different posts on various aspects of plantar fasciitis causes, symptoms and treatments. Here you'll find the overview summary with plenty of opportunities to learn more if you'd like.
Plantar Fasciitis Symptoms
The most common symptom of plantar fasciitis is pain under the heel. Either localised to just the heel or moving just slightly forwards into the arch.
The pain pattern for plantar fasciitis can be really interesting and unusual for those of us who have not had experience with soft tissue injuries in the past.
Typically a sharp pain or a pain like you've stepped on a stone will be felt on the first few steps when you get up. This could be first thing in the morning or after you've been sitting down for a while.
With a bit of walking and movement the pain levels tend to reduce, and for some can even disappear completely. Then, with more and more activity the pain can start to build again and feel like a burning or aching sensation under the foot.
It's very rare to have pain at rest or at night with plantar fasciitis.
Secondary symptoms relating to plantar fasciitis can affect the foot, ankle and lower leg. Often to compensate for our sore heel we'll start to walk more on our toes or on the outside of our feet. This can lead to pain around the ball of the foot, ankle and lateral calf.
Causes of Plantar Fasciitis
Plantar fasciitis is caused by asking the plantar fascia to do more than it can handle, repeatedly. There are three key concepts for us to understand here relating to overloading the fascia. First, we'll talk about capacity, and then we will talk about the types of load.
When Demand is Greater than Capacity
Every tissue in our body has the capacity to tolerate load. Think of a muscle or a bone. If you overload a muscle significantly it will get sore. If it's a one-off, it might be an ache or a strain. If it keeps happening there can be a significant tear. Bones too. The repeated loading of bones within their capacity keeps them strong. Tip-over into overload territory and bones start to develop stress responses and stress fractures.
The plantar fascia is no different. Load up your plantar aponeurosis and it will be happy and stay strong and stretchy. Overload it and you'll start to get excessive wear and damage to your fascia.
Things that can increase the capacity of your plantar fascia to tolerate load are being healthy, active and engaging with regular resistance training exercises. Good sleep and a good diet are also paramount. Younger folks have greater capacity in their connective tissues than older folks. So much so it's super rare for children to suffer from plantar fasciitis.
Inactive or sedentary lifestyles, stress, poor sleep, poor diet and older age all reduce the capacity of our plantar fascia to tolerate load. As does smoking, diabetes and recent antibiotic (some not all) usage.
Types of Load - Tension
There are two different types of load that our plantar fascia is placed under. Tension and compression. Tensile loading is the type of load our plantar fascia has evolved to handle. Think of a rubber band, pull it apart to place a stretch on the rubber. This is predominantly a tensile or pulling type load.
The plantar fascia cops this tensile loading each step. When we lower our foot to the ground the arch lowers as well pulling on the plantar fascia. This predominantly tensile load is taken up by the fibres of the plantar fascia. When we start to move forwards and lift our heel from the ground the tensile loading starts to reduce and we've received great arch support from our plantar aponeurosis.
When you think of how many steps we can take every day, it's an absolute mammoth amount of tensile load that is repeatedly placed on the plantar fascia.
Types of Load - Compression
Compression or compressive load is where instead of being pulled, things are pushed or squished together. Concrete and bone are two different materials that are exceptional at tolerating compression and thrive under this type of load.
The plantar fascia however does not like compression anywhere near as much as tensile loads. When we walk if we twist in or out at our heel bone, movements known as either inversion or eversion or sometimes supination or pronation we can place a compressive load on our plantar fascia.
What happens is if you tilt your heel significantly when you're walking and all your body weight is on one foot, the plantar fascia is compressed close to the heel bone. It does not take as much volume of this kind of load compared with the tensile load for the plantar fascia to complain and enter its overworked and overloaded state.
How Plantar Fasciitis is Diagnosed
Plantar fasciitis is most commonly diagnosed in the clinic by your podiatrist. There are enough clinical signs and symptoms and various tests that can be performed to leave imaging as optional or not necessary in most cases.
During a clinical examination, your podiatrist will determine your risk factors from your history. This will include things like your medical history, medications, previous injuries or surgery. From there a physical examination will look at joint range and quality of movement, joint axis positioning, foot shape and function. A gait analysis will show movement patterns that can increase or decrease the load on your plantar fascia.
Muscle testing, particularly of the calf muscle unit can indicate if an imbalance or weakness is contributing to your injury. Tests like calf raise power and endurance are great indicators.
If there is more information required or potentially a couple of injuries happening at the same time then imaging can be useful. For example, it's quite common for both plantar fasciitis and a heel fat pad injury to occur at the same time.
The two kinds of imaging that are useful are magnetic resonance imaging (MRI) or ultrasound imaging. An MRI is able to show the plantar fascia and surrounding soft tissues as well as the heel bone itself.
Ultrasound imaging in the hands of a skilled sonographer can be exceptional at showing the quality of the plantar fascia. Signs such as the thickness of your fascia, small tears, scarring or vascular growth can be seen clearly on ultrasound imaging.
A modality that really doesn't help with most forms of heel pain and plantar fasciitis, in particular, are plain film X-rays. X-ray imaging is great at showing up bone pathology however heel pain is very rarely related to bone pathology and even when it is, as, in the case of a calcaneal stress fracture, these injuries are not likely to show on a plain film x-ray.
How Plantar Fasciitis is Treated
Effective treatment of plantar fasciitis is all about reducing the overload and increasing the capacity of your plantar fascia.
We've written a detailed post on plantar fasciitis treatment here so this will be a short recap.
To reduce the overload on your plantar fascia you can work with your podiatrist to identify your specific triggers and adjust accordingly. For many, this will involve strapping tape to alter the compression and tensile loads placed upon the plantar aponeurosis. Footwear is important too with some shoes increasing and others decreasing how hard your fascia works.
Orthotics are another proven effective treatment for plantar fasciitis. Ensuring your orthotics are right for you is paramount as in the past many orthotics have been prescribed to provide "arch support" however in some cases this can increase the compression on the plantar fascia. And now you're an expert on compression and how much your fascia hates it, you'll understand why these devices did not work in the past.
To increase the capacity of your plantar fascia to do work and tolerate load resistance training exercises are required. Calf raise programs that train up both your calf muscles as well as your plantar fascia with some little tweaks and modifications are a mainstay.
The 1-Per-Cent-ers
The bulk of effective plantar fasciitis treatment is the specific, targeted and effective use of strapping, orthotics, footwear and strength-based exercises. But, there are some 1%ers that can help too.
Therapeutic massage to the arch and calf muscle area can reduce symptoms in the short term. There's an increasing body of evidence for extracorporeal shock wave therapy for both pain relief and increased healing responses too. Dry needling may have a place to play in some cases of plantar fasciitis but probably (ok definitely) not all.
Heat or ice packs to the plantar fascia have been reported to be useful by some, and thoroughly not helpful to others. If you want to try either they are relatively low-risk options however should not replace the more effective treatments listed above.
The Invasive Options
There are two much more invasive treatment options for plantar fasciitis that have limited effectiveness with much more significant side effects. For this reason, these treatments are only to be considered if other treatment options are not having the desired results.
Injection therapy with cortisone can provide pain relief for cases of persistent plantar fasciitis. A corticosteroid injection can be used to provide a window of appropriate rehabilitation exercise therapy to proceed if the pain is too great. The risks or downsides are that cortisone injections only provide temporary relief, decrease the bone density of the surrounding foot bones and increase the risk of rupture of the plantar fascia.
Surgery for plantar fasciitis is very rarely required as active measures are very effective. If a surgical procedure is performed it will either involve removing and cleaning away excess scar tissue or fibromas or lengthening the plantar fascia. Known as a plantar fascia release. Very rarely is the plantar aponeurosis surgically cut completely due to the increased demands on the foot and leg muscles and subsequent risk of osteoarthritis.
Treatments that Don't Work
Calf stretching or calf stretches have been a mainstay of plantar fasciitis treatment by physical therapists for decades. We have increasing evidence that as a treatment, they don't work.
Certainly, a tight calf muscle does increase the load on the plantar fascia and contributes to plantar fasciitis. But completing a calf stretch does not release or cause the calf to be any less tight in the long term.
Having a tight calf is usually a sign that your calf is overworked, a nice way of saying not as strong as it needs to be. To increase your calf strength with an appropriate resistance training program you can increase the length of your calf via a process known as sarcomerogenesis. If you'd like to learn more about why stretching exercises don't help chronic plantar fasciitis and what exercises to do we have a post for you on that too.
Want to Know More About Plantar Fasciitis? Here's the Knitty-Gritty Referenced Details
Plantar fasciitis healing times vary from person to person greatly. When picked up and treated early then the pain can be resolved almost immediately with strapping, taping, shoes or orthotics. From there the rehabilitation exercises tend to be required for 4 - 6 weeks minimum to increase the capacity of your plantar fascia.
If your plantar fasciitis has been building and sore for a longer period of time then healing times are longer. While it's common for pain relief quite quickly with appropriate treatment, prevention of recurrence does take a bit more time commitment to stick with your exercise program.
The same goes for those who have some comorbidities. If you have diabetes, are a smoker or perhaps had a few more birthdays under your belt the treatment timeframe is longer.
Wearing the right shoes for your feet is an integral part of recovering from plantar fasciitis. Check out our guide on the best shoes for plantar fasciitis to learn more.
Wearing high heels does not increase the tensile load on your plantar fascia compared with being barefoot or in flats, however, some other changes can occur.
With long term and consistent high heel use, the calf muscle unit can become shorter and weaker. This then leads to the increased loading on the plantar fascia and can contribute to plantar fasciitis.
For us podiatrists, we're mindful of just how important high heels can be to our mood and confidence. We might occasionally recommend adjustments to when or how often high heels are worn but it's not common we're completely against wearing power heels when needed.
The internet is a cesspit of home remedies and snake oil for plantar fasciitis but there are some things you can do at home that work exceptionally well.
Wearing the right shoes at the right time.
Exercises to increase the capacity of your plantar fascia and calf muscle unit.
Getting enough sleep and a healthy diet.
We’ve put together a guide on how to treat plantar fasciitis at home for you.
In most cases, running is an important activity for our overall health, both physical and mental. With your plantar fascia working harder when you run, it's also something that we have to be careful of when treating plantar fasciitis.
When you have a discussion with your podiatrist to set your treatment goals establishing a running program will be paramount for those who enjoy a run.
For most of us, modifying running volume in the short term slightly allows us to keep running whilst we treat our plantar fasciitis. It goes without saying that in these cases being absolutely specific and on board with any other exercises, shoe changes, strapping and orthotics are important too.
Plantar fasciitis will not go away on its own. The pain may increase or decrease due to natural variations in activity and footwear however completely treatment program is still needed to resolve and prevent recurrence.
Gel heel inserts may feel comfortable when first used however they do not have much of a place in effective plantar fasciitis treatment. They didn't even make it into the list of 1%ers. If you have foot pain the best course of action is to see your podiatrist for assessment, diagnosis and appropriate physical therapy.
Those of us with flat feet have just as much chance as those with high arches of getting plantar fasciitis. Flat feet tend to place more tensile load on the plantar fascia (which the fascia loves) whereas high arched feet compressive the fascia more.
Because of these variations in load types both can suffer with heel pain and effective treatment of plantar fasciitis via shoe inserts and exercises needs to be targeted to your exact needs.
A heel spur is a very normal thing for us to develop. For most of us the chance of having a heel spur is pretty much in line with our age... As in, 30% of people in their 30's and 60% of people in their 60's have heel spurs.
But, and this is a big but.
Having a heel spur is not likely to be painful or causing plantar fasciitis. Heel spurs can contribute to a rare condition known as Baxter's nerve entrapment but for almost all of us with bone spurs are not a problem.
The best analogy we can give is that bone spurs on the heel are like wrinkles on our face. They are normal changes that happen as we age. Some of us might not like the look of our heel spurs if we X-ray them (another reason why we don't x-ray heels) however they don't actually cause us problems, much like our wrinkles...
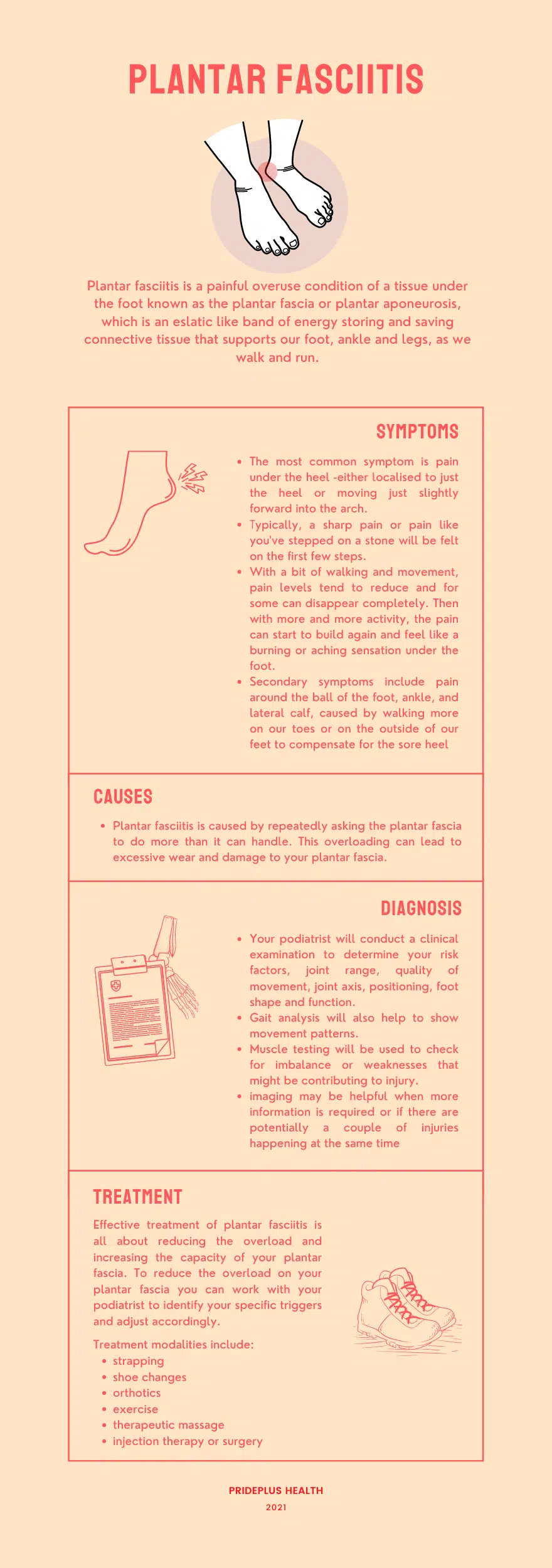
Plantar Fasciitis Infographic
Other Plantar Fasciitis Resources
- Online Heel Pain Diagnosis Test
- How To Treat Heel Pain at Home
- Interview with Dr Whittaker about Orthoses for Plantar Heel Pain
- Plantar Fasciitis Treatment
- Orthotics for Plantar Fasciitis
- The Best Shoes for Plantar Fasciitis
- Can Socks Help Plantar Fasciitis
High-load strength training improves outcomes in patients with plantar fasciitis: A randomised controlled trial with 12-month follow up. Scandinavian Journal of Medicine and Science in Sports. (2014). Rathleff M, Molgaard C, Fredburg U, Kaalund S, Anderson K, Jensen T, Aaskov S & Olesenj.
The association between pain catastrophising and kinesiophobia with pain and function in people with plantar heel pain. The Foot (Edinb.) 2017. Cotchett M, Lennecke A, Medica VG, Whittaker GA, Bonanno DR.
Long-Term Prognosis of Plantar Fasciitis: A 5- to 15-Year Follow-up Study of 174 Patients With Ultrasound Examination. Orthopaedic Journal of Sports Medicine (2018). Liselotte Hansen, Thøger Persson Krogh, Torkell Ellingsen, Lars Bolvig, and Ulrich Fredberg
Effectiveness of Trigger Point Dry Needling for Plantar Heel Pain: A Randomized Controlled Trial. Physical Therapy (2014). Cotchett M & Munteanu S.

About The Author
Tim Mulholland is a passionate podiatrist and clinical academic. For more than 10 years he has been helping clients every week understand and overcome their plantar fasciitis in the clinic. When not consulting he has spent 8 plus years teaching podiatry at La Trobe University where musculoskeletal disorders of the foot and ankle, as well as effective communication and goal setting, are key interests.



